Revenue Cycle Management (RCM) explained end to end—front, mid, and back office. Reduce denials, speed cash flow, track KPIs, and leverage AI. Get 2026 guide.

Healthcare organizations are at a crossroads. Patient call volumes are rising, but so are staffing shortages and employee burnout. This leads to long hold times, abandoned calls, and frustrated patients. Administrative teams are buried under repetitive phone calls to payers for benefits verification, prior authorizations, and claims status checks. These bottlenecks don’t just hurt the patient experience, they cause scheduling gaps and revenue leakage. This is where voice AI platforms compliant with healthcare regulations come in, with leading solutions like Prosper AI, Zocdoc’s Zo, and Luma Health offering a way to automate these crucial workflows securely and efficiently.
When we talk about compliance in healthcare AI, we’re referring to a strict set of rules designed to protect sensitive patient information. Generic AI platforms won’t cut it. A truly compliant solution must be built on a foundation of trust and security.
HIPAA (Health Insurance Portability and Accountability Act): This is the cornerstone of patient data protection in the United States. Any technology that handles protected health information (PHI) must be HIPAA compliant. This includes having technical, physical, and administrative safeguards in place.
BAA (Business Associate Agreement): A vendor that handles PHI on behalf of a healthcare provider must sign a BAA. This is a legally binding contract that requires the vendor to maintain HIPAA compliance and report any data breaches. Never use a platform that won’t sign a BAA.
SOC 2 Type II: This certification demonstrates that a company has robust internal controls for security, availability, processing integrity, confidentiality, and privacy over a period of time. It’s a critical trust signal for enterprise healthcare organizations.
Beyond the main frameworks, truly compliant platforms operate on key principles to safeguard data at every step.
Data Minimization: This principle dictates that organizations should only collect, use, or share the absolute minimum amount of PHI necessary to complete a specific task. This is crucial for AI, which often requires large data sets, ensuring that no superfluous information is accessed.
De-identification and Anonymization: These techniques are used to remove or obscure personal identifiers from datasets. De-identification strips away information like names and social security numbers, while anonymization goes further to transform data so it cannot be linked back to an individual. This allows AI models to be trained on valuable clinical data without compromising patient privacy.
Leading platforms are also adopting advanced computational techniques to enhance privacy. These “Privacy Preserving AI” methods allow for powerful analysis without exposing raw, sensitive data.
Federated Learning: Instead of pooling all data in one central location, federated learning trains AI models on decentralized data that remains secure within its original location, like a hospital’s server. Only encrypted model updates are shared, not the patient data itself, enabling collaboration without compromising privacy.
Differential Privacy: This technique adds a small, mathematically precise amount of statistical noise to a dataset. This noise is enough to protect any single individual’s identity while still allowing for accurate analysis of the overall data trends.
Homomorphic Encryption: A cutting edge method that allows AI to perform computations directly on encrypted data without ever needing to decrypt it first. This provides one of the strongest forms of data protection during processing.
When evaluating voice AI platforms compliant with healthcare regulations, use this checklist to ensure they meet essential security standards:
Signed BAA: A non negotiable requirement for any healthcare partner.
SOC 2 Type II Certification: Verifies long term, audited security practices.
HIPAA and GDPR Compliance: Ensures adherence to major data privacy regulations.
Data Encryption: Both in transit (TLS) and at rest (AES 256) to protect data from interception.
Secure User Access (SSO & MFA): Integration with providers like Google, Azure, or Okta for secure single sign on, fortified with multi factor authentication to prevent unauthorized access.
Secure Integrations: Safe connections to your EHR and PM systems through methods like REST APIs or SFTP.
Data Retention Policies: Clear policies on data handling, such as zero day retention agreements with underlying AI models like OpenAI.
Data Locality and Regional Processing: The ability to process and store data within specific geographic regions to comply with data sovereignty regulations.
Incident Response Plan: A documented strategy for how the vendor will respond to and mitigate the effects of a security breach, which is crucial for protecting patient safety and trust.
Secure Data Disposal: Formal policies and procedures for the irreversible destruction of PHI from electronic media when it is no longer needed, a key requirement of HIPAA.
Regular Security Audits: Includes vulnerability scans and third party penetration testing.
Choosing a compliant AI partner requires more than just checking boxes. It involves a thorough vetting process to confirm their commitment to security and privacy.
BAA Verification: Don’t just confirm they will sign a BAA. Review the terms to understand their responsibilities, breach notification protocols, and liability.
Comprehensive Risk Assessment: Your organization should conduct a risk assessment of any potential vendor. This involves evaluating their security posture, data handling practices, and the potential impact of a breach. Ask for their own third party audit reports and penetration test results.
Requesting Proof: Ask for copies of certifications like SOC 2 Type II reports. A trustworthy vendor will be transparent and provide the necessary documentation to validate their claims.
A voice AI platform is only as good as its ability to connect with your existing systems. Siloed data creates more work, defeating the purpose of automation. Your chosen platform must offer deep integration capabilities with major Electronic Health Record (EHR) and Practice Management (PM) systems.
Leading solutions provide 80+ EHR/PM integrations with vendors like Epic, athenahealth, Cerner, and NextGen. This relies on secure API integration, which uses modern authentication and encryption to create a safe bridge for data exchange. The goal is real time API connectivity, allowing the AI to instantly read patient data to make calls and, crucially, write structured results back into the patient record. This seamless data flow is essential for automating tasks like appointment scheduling and prior authorization follow up. If you’re considering voice AI platforms compliant with healthcare regulations, deep integration is a must have.
A fast time to value is critical. You shouldn’t have to wait six months to see a return on your investment. Top platforms can get you live with pilot programs using simple spreadsheets in just a couple of days. A full API integration should be achievable in under a month.
Effective governance includes AI powered quality assurance. Look for platforms that automatically review every single call for accuracy and compliance. This practice, known as call recording review, provides near real time analytics and allows you to benchmark AI performance directly against your human staff. One pharma hub found that AI QA accuracy actually outperformed their human teams in side by side reviews.
Implementing AI successfully also depends on patient trust. This is built through clear communication and respect for patient autonomy.
Patient Transparency: Be upfront with patients about when they are interacting with an AI. A simple disclosure like, “This call is being handled by our automated assistant,” can build trust and manage expectations.
Patient Consent: For many interactions, especially those involving the collection of new information, obtaining and documenting patient consent is a best practice and may be a legal requirement. Patients should understand how their data will be used and have the option to speak with a human agent.
How do you know if your voice AI is working? Track these key performance indicators (KPIs):
Call Abandonment Rate: Prosper AI customers have seen this drop by as much as 89%.
Patient Hold Times: The goal should be a zero second wait time for inbound calls.
Cost Per Call/Task: Look for cost reductions of 50% or more for tasks like benefits verification and claims follow up.
Appointment Volume: Proactive re engagement campaigns can increase scheduled appointments by 20% or more.
Denial Rate: Accurate, upfront benefits and authorization checks reduce costly denials.
Staff Satisfaction: Automating repetitive phone calls frees up staff for higher value, patient facing work, reducing burnout.
Now that we’ve established the critical importance of regulatory adherence in healthcare AI, it’s time to spotlight the platforms that are leading the charge. The following five voice AI solutions have been selected for their exceptional ability to blend advanced conversational technology with the stringent privacy and security standards required by regulations like HIPAA. These companies provide a blueprint for how to innovate responsibly, enhancing patient communication and administrative efficiency without compromising on data protection.
Prosper AI deploys specialized, phone agents that automate high-volume patient access and revenue cycle calls. Built for health systems, specialty groups, billing/RCM companies, and payors, it focuses on scheduling, eligibility/benefits, and billing questions to deliver immediate containment and relieve overwhelmed call centers.

Trust & compliance: HIPAA compliant with a BAA, SOC 2 Type II attestation, encryption in transit and at rest, and enterprise SSO with audit logging. Supports cloud and on prem/VPC deployments. Buyers should confirm PHI retention windows, redaction options, and data region controls.
Patient access: appointment scheduling, confirmations, reminders, and after hours coverage via voice and SMS.
RCM automations: benefits/eligibility verification, prior auth initiation/follow up, claims status, denial workflows.
Billing and IVR modernization: statement Q&A, payment capture, and conversational switchboard replacement with warm transfer.
Integrations: 80+ EHR/PM systems (Epic, athenahealth, Cerner), FHIR/APIs, SFTP, and PSTN/telephony.
Reported outcomes include 60%+ call containment and sharp abandonment reductions (e.g., ~89%). Typical time to value is 3 weeks with packaged workflows; pricing and BAA handled in procurement. Best fit for providers and RCM firms seeking fast containment on scheduling and billing lines.
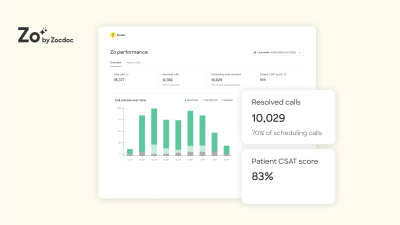
Zo is a voice first AI that answers unlimited inbound calls 24/7, understands natural language, and books directly into the EHR. It’s built for specialty groups, MSOs, and health system access centers aiming to convert more calls into completed appointments while reducing agent load.
Trust & compliance: Marketed as HIPAA compliant and SOC 2 certified, with BAA support. Data is encrypted in transit/at rest; role based access and possible SSO. Cloud only. Buyers should verify audit log granularity, transcript/recording retention, and data residency.
Patient access: end to end scheduling, reschedules, cancellations; insurance aware booking rules.
Switchboard/IVR: conversational routing with warm transfers to staff when needed; after hours coverage.
Outreach: captures peak volume and missed calls to reduce leakage and no shows.
Integrations: existing telephony plus 175+ EHR/PMS connections (Epic, athenahealth, Cerner, NextGen).
Vendors and case studies cite up to ~70% call containment and ~51% new patient conversion. Fast deployment and outcome based pricing make it a strong fit for appointment driven practices focused on access and conversion.
Luma Health’s Patient Success Platform is multimodal by design: voice for live calls, SMS for data collection, and web for follow through. Its Navigator voice AI handles inbound calls, pivots to text for insurance cards or forms, and writes results back to the EHR, ideal for enterprise health systems and large specialty groups seeking automation without losing continuity.

Trust & compliance: HIPAA with standard BAA; certified HITRUST, SOC 2 Type II, and ISO 27001. Encryption in transit/at rest, SSO, and audit logs are supported. Cloud based with a zero retention approach for model training. Confirm any optional retention/redaction settings.
Switchboard/IVR replacement: natural language call handling with intelligent transfers.
Patient access: scheduling updates, common FAQs, prescription refill requests; seamless SMS handoff for data capture.
Intake and payments: insurance card capture, copay collection, and form completion via text.
Integrations: bi directional support for Epic, Oracle Health (Cerner), MEDITECH, athenahealth, NextGen.
Customers report automating a large share of after hours calls (up to ~95% in some programs). Expect a weeks long rollout for targeted use cases. Strong fit for health systems prioritizing tight EHR write back and omnichannel journeys.
Hyro brings healthcare specific NLU to voice, SMS, and web channels to reduce hold times and deflect repetitive calls. It shines in large health systems and integrated provider networks by guiding patients through scheduling, refills, and billing support with consistent, channel agnostic experiences.
Trust & compliance: HIPAA compliant with reported SOC 2 posture and enterprise BAA support. Request details on current SOC 2 type, encryption standards, SSO/audit logs, PHI retention, and data residency for its cloud deployment.
IVR modernization: smart routing and high containment across voice and SMS.
Patient access: end to end appointment scheduling, prescription refills, reminders.
Revenue cycle: billing/registration Q&A and proactive outreach for coverage checks.
Integrations: Epic (App Orchard), Oracle Cerner, athenahealth, plus Cisco/Genesys for CCaaS/telephony.
Case studies cite ~65% call deflection, major abandonment reductions (~85%), and strong ROI. Good fit for switchboard offload and scheduling at scale, with deployments measured in days for proven flows.
Kore.ai’s platform powers voice, SMS, and chat with HealthAssist, a healthcare specific solution spanning patient access and RCM. It’s built for enterprise providers, specialty groups, RCM firms, and payors seeking broad automation, from scheduling to benefits and claims, with strong governance and deployment flexibility.

Trust & compliance: HIPAA compliant, SOC 2 Type II, and signs BAAs. End to end encryption, SSO, audit logs, and configurable PHI retention/redaction. Flexible hosting: public cloud, private cloud, or on prem. Verify data residency per region.
Patient access: appointment scheduling, reminders/recalls, after hours coverage across voice/SMS/chat.
RCM: eligibility/benefits verification, claims status/EOB retrieval, billing Q&A and payments.
Conversational IVR: intelligent routing, deflection, and contextual handoffs to live agents.
Integrations: FHIR/APIs into major EHR/RCM systems; CCaaS/telephony including Genesys and NICE.
Clients report high containment (often up to ~90%) and faster service with prebuilt healthcare flows. Time to value is typically weeks; strong choice for enterprises requiring governed, multi channel automation.
The applications for compliant voice AI in healthcare are vast, covering both patient access and revenue cycle management. For a deeper breakdown, explore our healthcare AI voice agent use cases.
AI Appointment Scheduling: AI agents can handle inbound scheduling requests 24/7, reducing front desk workload by 50% or more. A large Northeast GI group used AI to clear call backlogs and accelerate scheduling within weeks.
Switchboard Automation: Conversational AI can replace frustrating IVR menus, quickly routing patients to the right department.
Appointment Reminders: Automated calls and texts can reduce no show rates by around 30%.
Re engagement Campaigns: AI can proactively call patients who are overdue for preventative care, keeping provider schedules full.
Benefits Verification: AI agents call payers to verify eligibility and coverage, capturing dozens of data points with 99% accuracy in under two hours.
Prior Authorization: AI can initiate prior authorization requests and perform relentless follow up, reducing delays and denials.
Claims Status and Denial Follow up: AI agents check on claims over 30 days old and can even push back on payer errors, increasing collections on denied claims by 15%.
While most enterprise voice AI platforms do not list public pricing, the return on investment is clear and fast. Pricing is typically based on call volume and the specific use cases you deploy. The ROI comes from several areas:
Reduced Labor Costs: Automating phone calls can result in a 50% cost reduction compared to manual efforts.
Increased Revenue: Filling schedules, reducing no shows, and lowering denial rates directly boosts your bottom line.
Improved Staff Retention: By reducing burnout from repetitive tasks, you lower turnover and associated hiring costs.
With go live times as short as a few weeks, practices can quickly see significant operational and financial improvements, making the investment in voice AI platforms compliant with healthcare regulations a strategic advantage.
The world of voice AI is evolving rapidly. We can expect to see even more sophisticated conversational capabilities and deeper integrations. AI will become more proactive, not just reacting to inbound calls but anticipating patient needs and administrative requirements. As large language models become more efficient, the cost of these services will continue to fall, making them accessible to a wider range of healthcare organizations. The continued focus on security will ensure that even the most advanced voice AI platforms compliant with healthcare regulations remain a safe choice for providers.
The administrative burden in healthcare is unsustainable. Staff are overwhelmed, patients are frustrated, and revenue is lost. Voice AI platforms compliant with healthcare regulations offer a powerful solution. By securely automating high volume, repetitive phone calls for patient access and RCM, these platforms free up your team to focus on what matters most: patient care. They reduce costs, increase revenue, and create a better experience for everyone. When evaluating your options, prioritize platforms built specifically for healthcare that offer robust security, deep EHR integrations, and a proven track record of rapid time to value.
Ready to eliminate hold times and automate your front desk? Get started.
A platform is HIPAA compliant when it implements required physical, administrative, and technical safeguards to protect patient data. This is formalized through a signed Business Associate Agreement (BAA), which legally binds the vendor to protect PHI according to HIPAA rules.
Advanced AI voice agents are trained on thousands of real calls with payers. They learn to navigate interactive voice response (IVR) menus, wait on hold patiently, and converse with human agents to get the information needed for tasks like benefits verification or prior authorization status checks.
Implementation time varies. A pilot program using batch data, like a spreadsheet, can go live in as little as one or two days. A full integration with an EHR system typically takes about three weeks with a dedicated platform like Prosper AI.
Yes, leading voice AI platforms compliant with healthcare regulations provide no code tools. These allow your own operations teams to easily edit call scripts and workflows without needing any programming knowledge, ensuring the AI aligns perfectly with your processes.
Healthcare providers typically see a significant ROI driven by a 50% reduction in costs for phone based tasks, a 20% or more increase in scheduled appointments, and a 15% higher collection rate on denied claims. This is in addition to improved patient satisfaction and reduced staff burnout.
No, there are significant differences. Many generic platforms lack the specific training for healthcare conversations, deep EHR integrations, and the necessary compliance certifications like SOC 2 Type II. It is crucial to choose a vendor that specializes in the healthcare industry.
Discover how healthcare teams are transforming patient access with Prosper.
Revenue Cycle Management (RCM) explained end to end—front, mid, and back office. Reduce denials, speed cash flow, track KPIs, and leverage AI. Get 2026 guide.

Learn payer verification best practices to cut denials, speed reimbursement, and boost patient transparency. See steps and 2026-ready workflows you can use.

Learn how AI for Revenue Cycle Management automates prior auths, boosts clean claims, cuts denials, and accelerates cash flow. Get the 2026 guide and roadmap.