Evaluate HIPAA-compliant voice AI providers 2025: top 5 picks, security and SLA checklists, EHR integrations, KPIs, and rollout tips. Get the buyer’s guide.
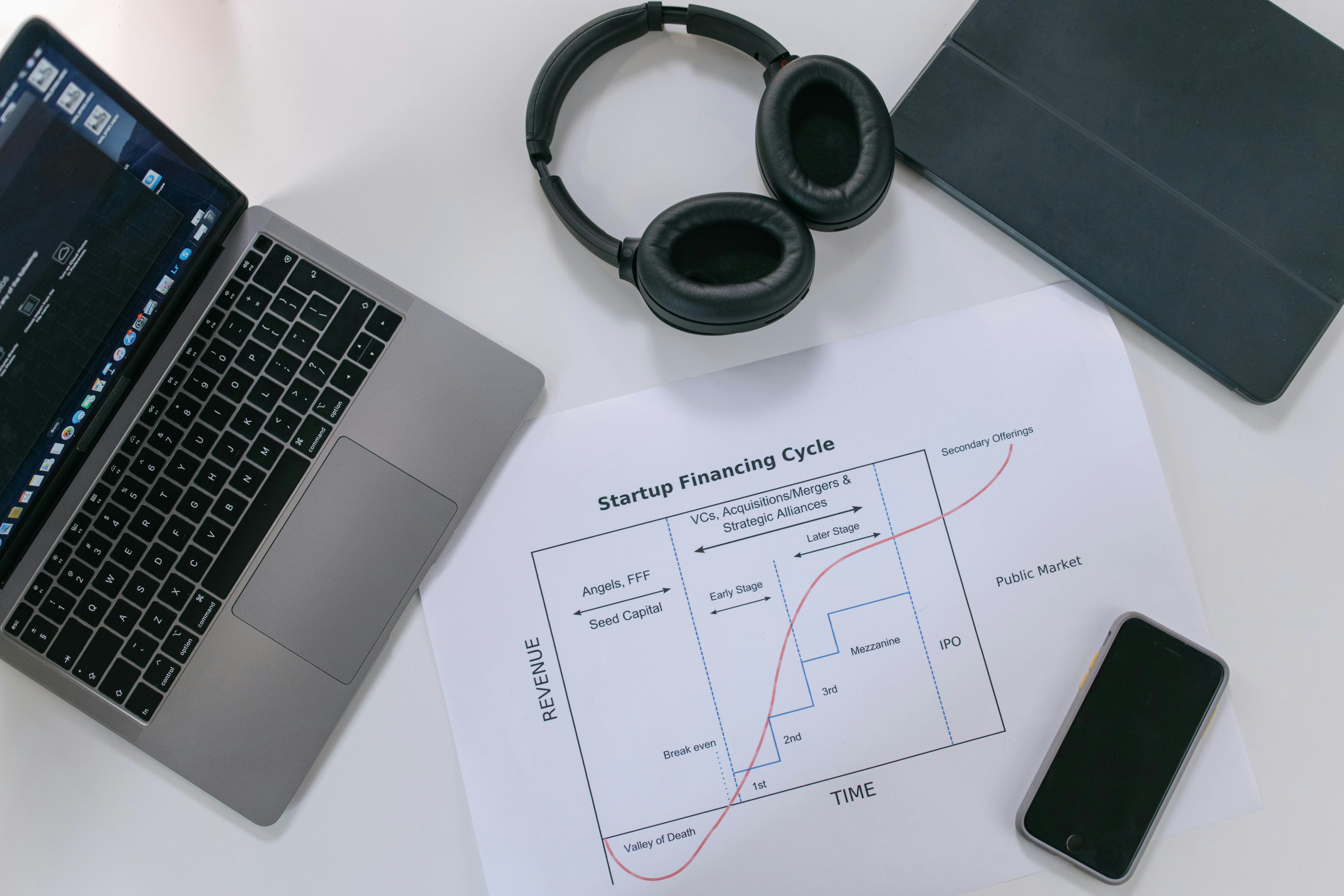
Revenue cycle management, often called RCM, is the financial backbone of any healthcare organization. Think of it as the entire journey of a patient’s account, from the moment they schedule an appointment to the moment their bill is fully paid. It’s a complex process that connects the clinical side of healthcare (treating patients) with the business side (getting paid for it).
In the U.S. healthcare system, where providers submit a staggering $3 trillion in claims each year, having a smooth and efficient revenue cycle management process isn’t just a nice to have, it’s essential for survival. A strong RCM system ensures healthy cash flow, minimizes lost revenue, and ultimately allows providers to focus on what they do best: patient care.
The RCM process isn’t a single action but a series of connected steps. A mistake at the beginning can cause major headaches at the end. Let’s walk through the key components of revenue cycle management.
This is where a successful revenue cycle begins. Getting things right at the front end prevents a huge number of problems down the line. In fact, a staggering 41% of all claim denials can be traced back to errors made during these initial steps.
The cycle kicks off when a patient books an appointment. Patient pre registration is the process of gathering key demographic and insurance details before the patient ever steps foot in the office. This is followed by patient registration and scheduling, which captures any remaining details when the appointment is officially booked or at check in.
Accurate data entry here is critical. Simple mistakes like a typo in a name or an incorrect insurance ID are a leading cause of claim denials.
Before providing a service, you need to know if the patient’s insurance will cover it. Insurance verification and eligibility is the process of checking with the payer to confirm the patient has an active policy, what their benefits cover, and what their out of pocket costs (like copays and deductibles) will be.
Failing to do this is a huge financial risk. Registration and eligibility errors alone account for nearly 27% of all medical claim denials. Manually calling insurance companies to verify benefits is a time consuming task that bogs down staff. This is where modern solutions can make a massive impact. AI powered voice agents can automate these calls, getting complete benefits information in hours with 99% accuracy and freeing up your team for more complex tasks.
Once the patient has been seen, the focus shifts to translating the clinical services into a bill that can be sent to the insurance company.
Charge capture is the process of recording every single billable service and item, from the doctor’s time to a surgical implant or medication. Missing a charge means losing revenue. One hospital, after implementing better tracking, found it was capturing 127% more billable value from OR supplies that were previously being missed.
Next, medical coding translates those services and diagnoses into universal codes using systems like ICD-10 and CPT. This is a highly specialized skill, especially since the ICD-10 system contains around 68,000 diagnosis codes. An incorrect code can lead to a denial or an underpayment.
With all the information gathered and coded, the claim is submitted to the payer, usually electronically. The payer then puts the claim through adjudication, a review process to check for accuracy and coverage. If the claim is “clean” (meaning it has no errors), it gets approved for payment. However, denial rates have been on the rise, with private insurers denying around 11% of claims in recent years.
This final stage is all about managing payments, dealing with denials, and collecting what’s owed from patients.
When a claim is denied, the work isn’t over. Denial management and appeal is the crucial process of investigating why a claim was rejected, fixing the issue, and formally appealing the payer’s decision. This is a massive opportunity for revenue recovery. While the average initial denial rate hovers around 12%, it’s estimated that nearly 85% of these denials are actually preventable or fixable.
The problem is that reworking a denied claim is expensive, costing anywhere from $25 to $181 in administrative time. Because of this, many denied claims are never appealed, leading to permanently lost revenue. Yet the effort pays off, as over 60% of appealed claims are ultimately paid. Automating this follow up is a game changer for many organizations. AI powered denial follow up solutions from Prosper AI can call payers, argue denials, and track statuses, helping providers collect up to 15% more on appealed claims at a fraction of the manual cost. See our case studies.
Once a payer approves a claim, they send payment along with a remittance advice, which explains what was paid and what adjustments were made. Remittance processing and payment posting involve applying these payments and adjustments to the correct patient accounts. Revenue reconciliation is the final check to ensure the money expected matches the money received across the entire organization, flagging any discrepancies for investigation.
After the insurance company pays its portion, the remaining balance is the patient’s responsibility. Patient billing and collection involves sending statements and collecting these out of pocket costs. With rising deductibles, this has become a huge challenge. Over 100 million people in America have healthcare debt, and medical bills are the most common type of debt sent to collection agencies. Clear, compassionate financial communication and flexible payment options are key to improving patient collections.
The end goal for every account is medical account resolution, which means the balance is zero. This happens through full payment from insurers and patients, or through other means like financial assistance write offs. The faster accounts are resolved, the healthier the organization’s cash flow.
A successful revenue cycle management strategy isn’t just about executing the steps, it’s about continuously measuring and improving them.
Beyond daily operations, several high level factors shape RCM success.
Effective RCM is also deeply connected to the patient experience and ethical considerations.
A team of dedicated professionals is required to manage the complexities of the revenue cycle.
To truly understand revenue cycle management, it helps to clear up a few common myths.
Ultimately, effective revenue cycle management is what allows a healthcare organization to remain financially viable so it can continue serving its community. It plugs revenue leaks, accelerates cash flow, ensures regulatory compliance, and improves the patient financial experience. In an industry of thin margins, optimizing every step of the revenue cycle isn’t just a business strategy, it’s a mission critical function that supports the delivery of high quality care. Ready to explore AI-driven RCM automation for your organization? Get started.
The primary goal of revenue cycle management is to efficiently and accurately collect the maximum possible revenue for services provided, as quickly as possible. This ensures the financial stability and sustainability of the healthcare organization.
The RCM process can be broken down into three main stages:
Denial management is critical because a significant portion of healthcare claims are initially denied by payers. Without a strong process to appeal these denials, providers would lose a substantial amount of revenue. Since many denials are correctable, an effective denial management program can recover millions of dollars that would otherwise be lost.
AI and automation can dramatically improve revenue cycle management by taking over repetitive, time consuming manual tasks. AI voice agents can handle phone calls to payers for benefits verification, prior authorization, and claim status checks, freeing up staff to focus on more complex issues. This reduces administrative costs, speeds up processes, and decreases errors, leading to faster payments and fewer denials.
A “clean claim” is a medical claim that is submitted to an insurance company with no errors or missing information. These claims can be processed and paid quickly without needing to be corrected or resubmitted, which is the ideal outcome in the RCM process.
Revenue cycle management is a shared responsibility across multiple departments. While a Director or Manager of Revenue Cycle oversees the process, it involves front desk staff (for registration), clinicians (for documentation), coders, billers, and the finance department. Everyone plays a role in ensuring the cycle runs smoothly. For additional common questions about our platform and approach, visit our FAQ.
Discover how healthcare teams are transforming patient access with Prosper.

Evaluate HIPAA-compliant voice AI providers 2025: top 5 picks, security and SLA checklists, EHR integrations, KPIs, and rollout tips. Get the buyer’s guide.
Learn how to build HIPAA-compliant AI frameworks 2025 with BAAs, least-privilege, RAG, and zero retention. Get a clear, actionable roadmap. Download the guide.

Learn what a patient scheduler does, key skills, pay, and paths to get hired. See duties, tools, and AI trends—plus tips to stand out. Read the complete guide.