Evaluate HIPAA-compliant voice AI providers 2025: top 5 picks, security and SLA checklists, EHR integrations, KPIs, and rollout tips. Get the buyer’s guide.

Artificial intelligence is transforming healthcare, promising to streamline everything from patient scheduling to medical billing. But as this powerful technology enters the clinic, it runs headfirst into a critical roadblock: the Health Insurance Portability and Accountability Act, or HIPAA. For any healthcare organization, from health systems to medical billing companies, looking to innovate, understanding the rules for hipaa compliant ai is a legal and ethical necessity. An AI solution becomes HIPAA compliant when it is governed by a Business Associate Agreement (BAA) and incorporates specific technical, physical, and administrative safeguards to protect patient data.
Generative AI, like the large language models that power advanced chatbots, can summarize doctor’s notes, handle patient inquiries, and automate tedious administrative tasks. However, the moment these tools touch Protected Health Information (PHI), they fall under HIPAA’s strict privacy and security standards. This guide breaks down exactly what you need to know to leverage AI’s power safely and effectively.
Before you can deploy an AI solution, you have to grasp a few non negotiable concepts. AI is not automatically compliant. Compliance depends entirely on how the technology is built, implemented, and managed by both the healthcare provider and the AI vendor. The introduction of AI doesn’t change HIPAA’s foundational rules, but it does require a modern interpretation of them.
HIPAA is built on several key rules, but the Privacy and Security Rules are most relevant to AI.
The Privacy Rule governs the use and disclosure of PHI. For AI, this means ensuring systems only access the “minimum necessary” information required for a specific task.
The Security Rule dictates the safeguards needed to protect electronic PHI (ePHI). For AI, this requires robust technical controls like encryption, access controls, and detailed audit logs to track who accesses data and when.
The Breach Notification Rule requires organizations to notify patients and authorities if unsecured PHI is breached. AI systems must be capable of detecting and reporting these incidents promptly.
Let’s get this out of the way: the public version of ChatGPT is not HIPAA compliant for handling patient data. Standard consumer AI tools often use the data you input to train their models, which is a direct violation of HIPAA’s confidentiality rules. A healthcare provider cannot simply paste a patient’s medical notes into a public AI and remain compliant.
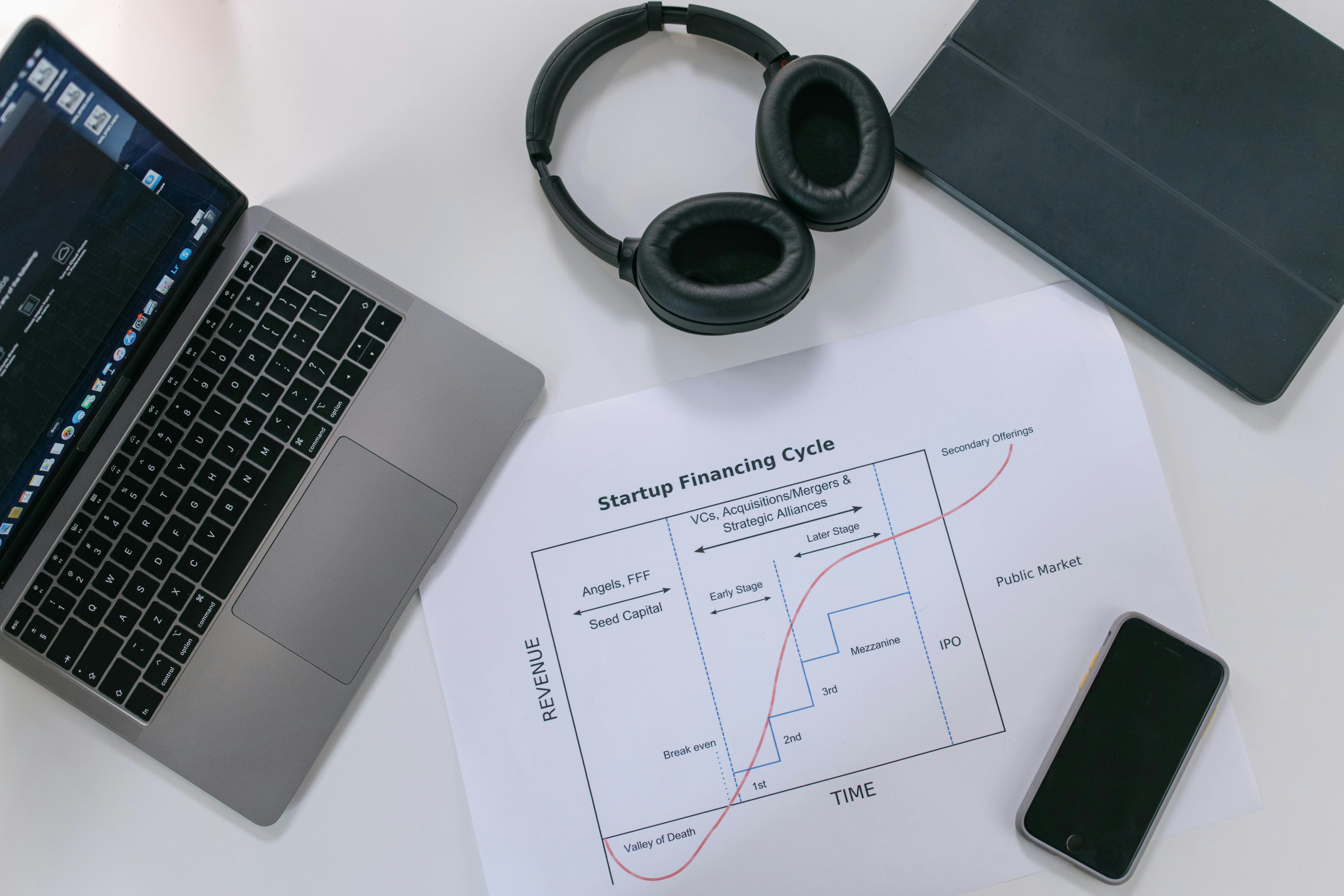
However, enterprise level AI services are a different story. Major providers like Google, Microsoft, and OpenAI now offer specific platforms (like Azure OpenAI Service or Google’s Med PaLM 2) that are designed for regulated industries. These services can be part of a HIPAA‑compliant AI strategy for patient access and revenue cycle workflows, but only when used under a crucial legal agreement.
The single most important document in this process is the Business Associate Agreement (BAA). A BAA is a legally binding contract required by HIPAA whenever a vendor (a “business associate”) handles PHI on behalf of a healthcare provider (a “covered entity”).
If an AI vendor processes PHI for you, they are a business associate, and you must have a signed BAA with them. This contract obligates the vendor to:
Safeguard patient data with appropriate security measures.
Use PHI only for the purposes specified in the contract.
Report any security incidents or data breaches to you.
Acknowledge their legal liability for any violations.
Failing to secure a BAA before sharing PHI is a serious violation. In one enforcement action, a healthcare practice was fined $31,000 for disclosing thousands of patient records to a vendor without a BAA in place. When vetting a partner for hipaa compliant ai, if they can’t or won’t sign a BAA, the conversation is over.
HIPAA is not designed to stop the flow of health information, but to channel it appropriately. Understanding when AI can use PHI and when it needs explicit patient permission is critical.
HIPAA allows covered entities and their business associates to use and share PHI without patient authorization for essential activities defined as Treatment, Payment, and Healthcare Operations (TPO).
Treatment: An AI tool that analyzes a patient’s chart to help a clinician determine the best course of action falls under treatment.
Payment: Using an AI agent to verify a patient’s insurance benefits or check the status of a claim is a payment activity.
Operations: Deploying AI to schedule appointments or conduct quality assessments is considered a healthcare operation.
A compliant AI tool can perform these TPO functions with PHI, provided it operates under a BAA and adheres to the minimum necessary standard.
Using PHI for purposes that fall outside of TPO generally requires written authorization from the patient. A primary example is using patient data to train a new AI model. Since model training is not considered a TPO activity, you must get explicit consent from each patient whose data will be used.
A valid consent process should be transparent and clear, explaining what data will be used, for what purpose, and how it will be protected. Patients must also have the right to opt out without affecting their quality of care.
Once the legal framework is in place, compliance shifts to how the AI system actually handles sensitive data. The best systems are built with privacy as a default setting, not an afterthought.
The safest way to use health data with AI is to strip it of all personal identifiers first, a process called de-identification. Under HIPAA, properly de identified health information is no longer considered PHI.
However, AI introduces new challenges. Advanced algorithms can analyze large, supposedly anonymous datasets and link them with publicly available information to re identify individuals. This is known as data triangulation. One study found that 99.98% of Americans could be re identified using just 15 demographic attributes. Because of this risk, it is crucial to use robust de identification methods and include contractual prohibitions against any attempts to re identify data.
Two core principles should guide your data strategy for a hipaa compliant ai system:
Data Minimization: An AI should only access the absolute minimum amount of PHI necessary to perform its task. If an AI agent is scheduling an appointment, it needs the patient’s name and desired time, not their entire medical history. This “minimum necessary” rule is a bedrock principle of HIPAA.
Data Retention: Don’t hoard PHI. A clear data retention policy should define how long data is stored before it’s securely deleted. The longer you keep sensitive data, the longer it’s at risk. For example, some top tier AI vendors offer a zero day retention policy, meaning patient data is purged immediately after a task is completed, ensuring it isn’t stored on the AI provider’s servers.
A critical question to ask any AI vendor is whether they use your data to train their models. Using PHI to train general AI models that serve other clients is a major HIPAA violation unless you have explicit patient authorization. A truly hipaa compliant ai vendor will contractually guarantee that your data is never used for model training.
You should also have a clear policy on data residency, which dictates the geographic location where data is stored. While HIPAA doesn’t mandate that data stay in the U.S., many healthcare organizations require it contractually to simplify legal jurisdiction and compliance.
Whether you are developing an AI tool in house or purchasing one from a vendor, the architecture of the application itself must be built for security and privacy.
A well-designed AI application bakes HIPAA requirements into its very foundation, a concept you can see in action with the Prosper AI platform. This “privacy by design” approach includes several key technical safeguards.
HIPAA Compliant User Registration: The user signup process must be secure. It should collect only the minimum necessary information, transmit it over encrypted connections (like HTTPS), and enforce strong password policies. Multi factor authentication (MFA) is quickly becoming a standard and is highly recommended.
Access Control: Only authorized users should be able to access PHI. A robust system uses unique user IDs and role based access control (RBAC), ensuring a nurse can only see her patients’ data and a billing specialist can’t access clinical notes.
Encryption at Rest and In Transit: All PHI must be unreadable to unauthorized parties. This means using strong encryption like AES 256 for data stored in databases (“at rest”) and TLS for data sent over networks (“in transit”).
Audit Logging and Monitoring: The system must keep a detailed log of who accessed PHI, what they did, and when they did it. These audit logs must be regularly monitored to detect suspicious activity, like an employee accessing records they shouldn’t or an account downloading data at odd hours.
Choosing the right technology partner is one of the most important steps in implementing hipaa compliant ai. Your due diligence process, or vendor vetting, should be thorough.
Ask About Security: Go beyond the BAA. Ask for details about their security program, encryption standards, and access controls.
Look for Certifications: While there is no official government HIPAA certification, look for third party attestations like a SOC 2 Type II report or HITRUST CSF certification. These show that a vendor has undergone a rigorous independent audit of their security controls. For example, leading platforms like Prosper AI maintain SOC 2 Type II certification to demonstrate their commitment to enterprise grade security. You can review a recent healthcare AI case study to see the impact in practice.
Review Privacy Policies: A vendor’s privacy policy should be transparent and clearly explain how they handle data, including what information is collected, how it’s used, and whether it’s shared with third parties.
Understand Data Handling: Clarify their policies on data retention, model training, and data residency to ensure they align with your organization’s compliance requirements.
HIPAA compliance isn’t a one time setup; it’s an ongoing process of vigilance, training, and adaptation.
Technology alone can’t ensure compliance. Your team is your first line of defense. All staff who interact with the AI system must be trained on its proper use and your organization’s HIPAA policies.
The HIPAA Compliance Officer plays a central role in any AI project. This individual or team must be involved from the beginning to conduct risk assessments, vet vendors, develop policies, and oversee implementation and ongoing audits.
It’s important to recognize that HIPAA doesn’t cover all health information. Many wellness apps, fitness trackers, and other direct to consumer digital health tools fall outside of HIPAA’s jurisdiction. This has created a regulatory gap that the Federal Trade Commission (FTC) is actively filling.
The FTC’s Health Breach Notification Rule (HBNR) requires non HIPAA covered entities to notify consumers, the FTC, and sometimes the media following a breach of personal health record information. The FTC has recently expanded the rule to explicitly cover health apps and similar technologies. Critically, the FTC considers the unauthorized sharing of health data, such as with an advertising company without user consent, to be a “breach” that triggers notification requirements. This makes it essential to understand the data practices of any health technology, even those not directly governed by HIPAA.
Imagine an AI voice agent that handles patient scheduling and benefits verification calls, which are workflows common across health systems. To be a hipaa compliant ai solution, this agent must operate under a strict set of rules.
The BAA: The vendor providing the agent, like Prosper AI, must sign a BAA with the hospital.
Secure Operations: Every call is encrypted. The AI only accesses the patient data needed to schedule the appointment or check benefits. All actions are logged for auditing.
Data Control: After the call, the structured results are written back to the EHR through Prosper’s 80+ EHR and practice‑management integrations, and the sensitive PHI from the interaction is not retained by the AI’s core model, preventing data leakage or misuse in training.
Vendor Trust: The vendor has a SOC 2 report, proving its security controls are consistently effective.
This is how a hipaa compliant ai system works in the real world. It combines legal agreements, technical safeguards, and operational discipline to deliver value without compromising patient privacy. To see how these principles come to life, you can request a demo of Prosper AI’s voice agents.
Yes, absolutely. HIPAA does not prohibit the use of any specific technology. It simply requires that if a technology is used to handle PHI, it must be done in a way that complies with the Privacy and Security Rules.
The single most important step is ensuring you have a signed Business Associate Agreement (BAA) with any AI vendor that will access, process, or store PHI on your behalf. Without a BAA, sharing PHI with a vendor is a violation.
No. Public versions of AI tools are generally not HIPAA compliant because they do not offer a BAA and may use your input data for model training, which violates patient privacy. You must use an enterprise‑grade AI service that is specifically offered under a BAA. For a side‑by‑side overview of compliant options, see our guide to voice AI platforms compliant with healthcare regulations.
The difference isn’t in the core technology but in the implementation and legal framework around it. A hipaa compliant ai solution is one that is deployed with all the required safeguards (encryption, access controls, audit logs) and is governed by a BAA that contractually obligates the vendor to protect PHI according to HIPAA standards.
Vendors demonstrate their commitment to compliance through several means: readily signing a BAA, achieving third party security certifications like SOC 2 Type II or HITRUST, and providing clear documentation on their security architecture and data handling policies.
No. HIPAA compliance is a shared responsibility. While a compliant vendor provides the secure foundation, your organization is still responsible for using the tool correctly, managing user access, training your staff, and following HIPAA’s administrative requirements.
Discover how healthcare teams are transforming patient access with Prosper.

Evaluate HIPAA-compliant voice AI providers 2025: top 5 picks, security and SLA checklists, EHR integrations, KPIs, and rollout tips. Get the buyer’s guide.
Learn how to build HIPAA-compliant AI frameworks 2025 with BAAs, least-privilege, RAG, and zero retention. Get a clear, actionable roadmap. Download the guide.
Learn the full revenue cycle management process, from intake to coding, claims, denials, and patient billing—plus KPIs and AI tips. Boost cash flow today.