Evaluate HIPAA-compliant voice AI providers 2025: top 5 picks, security and SLA checklists, EHR integrations, KPIs, and rollout tips. Get the buyer’s guide.

In healthcare, the phone is a lifeline. It’s how patients schedule appointments, ask about bills, and get answers to urgent questions. But that lifeline is often stretched thin. Patients face long hold times, staff juggle endless calls, and simple tasks become major bottlenecks. The solution is to automate healthcare calls by implementing conversational AI that integrates with core systems like your EHR to handle routine, high volume tasks. This approach creates a more efficient and patient friendly experience.
Modern health systems and hospitals are discovering that to successfully automate healthcare calls isn’t about replacing humans with robots. It’s about empowering your team by letting technology handle the repetitive, time consuming tasks. This guide walks through everything you need to know to automate healthcare calls, from scheduling and billing to the technology that makes it all possible.
The traditional call center model is struggling to keep up, which is why it’s so important to automate healthcare calls. Staffing shortages and burnout are common, while patient expectations for instant service are rising. Let’s look at the core challenges automation solves.
Patient needs don’t stick to a 9 to 5 schedule. A significant number of appointment requests, around 70%, happen after hours. Yet, only 19% of healthcare call centers offer round the clock service. This gap leads to missed opportunities and delays in care. An AI voice agent can provide 24/7 availability, answering calls instantly day or night to schedule appointments or provide information, ensuring no patient call goes unanswered.
In specialty group practices, a typical call center can field 2,000 calls per day. During peak hours, this volume can easily overwhelm staff, leading to an average hold time of 4.4 minutes. Considering about two thirds of patients will hang up after waiting just two minutes, that’s a lot of lost connections. When you automate healthcare calls, you introduce incredible scalability. AI agents can handle hundreds of calls simultaneously with zero hold time, a feat impossible for human teams. This capability can lead to an 89% reduction in abandoned calls, ensuring more patients get the help they need right away.
The first and most impactful step for patient access use cases is to automate healthcare calls for patient facing communication. It directly improves the patient journey from their very first interaction.
A “digital front door” refers to all the technologies a provider uses to engage with patients digitally. By automating key phone based touchpoints, you create a cohesive and accessible entry point to your practice. This strategy meets patients where they are, offering convenient, self service options that streamline their entire healthcare journey, from scheduling to follow up.
Booking appointments over the phone is still incredibly common, accounting for as many as 88% of all scheduled visits. This manual process is a major source of administrative work and patient wait times. With appointment scheduling automation, an AI agent can greet a patient, check a provider’s real time calendar through EHR integration, offer available slots, and book the appointment directly. This streamlines the process and gives patients the convenience they want. Platforms like Prosper AI use AI agents like “Anna” to handle these calls, freeing up front desk staff to focus on patients in the clinic.
Effective patient engagement is crucial for better health outcomes and loyalty. Automation moves communication from being reactive to proactive.
Appointment Reminders and Follow up: Missed appointments cost the U.S. healthcare system a staggering $150 billion annually. Automated calls and texts for appointment reminders have been shown to reduce no show rates by about 30%. Automation can also handle post visit follow up, checking on patients after a procedure or reminding them to schedule their next checkup, closing care gaps and improving outcomes.
Test Result Notification: Instead of waiting for a nurse to call, an automated system can securely notify patients when their lab results are ready. For normal results, the AI can deliver the information directly. For results requiring discussion, it can prompt the patient to schedule a follow up appointment, reducing patient anxiety and freeing up clinical staff.
Nothing frustrates a caller more than being transferred multiple times. In healthcare, transfer rates can be as high as 19%, meaning nearly one in five patients gets bounced around. Smart call routing and triage solve this.
Conversational IVR: Instead of a confusing “press 1 for…” menu, a conversational AI can ask, “How can I help you today?” and understand the caller’s intent.
Voicemail Transcription: For after hours calls or when lines are busy, AI can transcribe voicemails into structured text, allowing staff to quickly triage and respond to patient needs without listening to messages one by one.
Nurse Triage Support: For clinical calls, an AI agent can perform initial intake by collecting patient demographics and symptoms based on established protocols. It then routes the call, along with a summary of the information, to a live nurse for assessment, ensuring urgent cases are prioritized and nurses have context before the conversation begins.
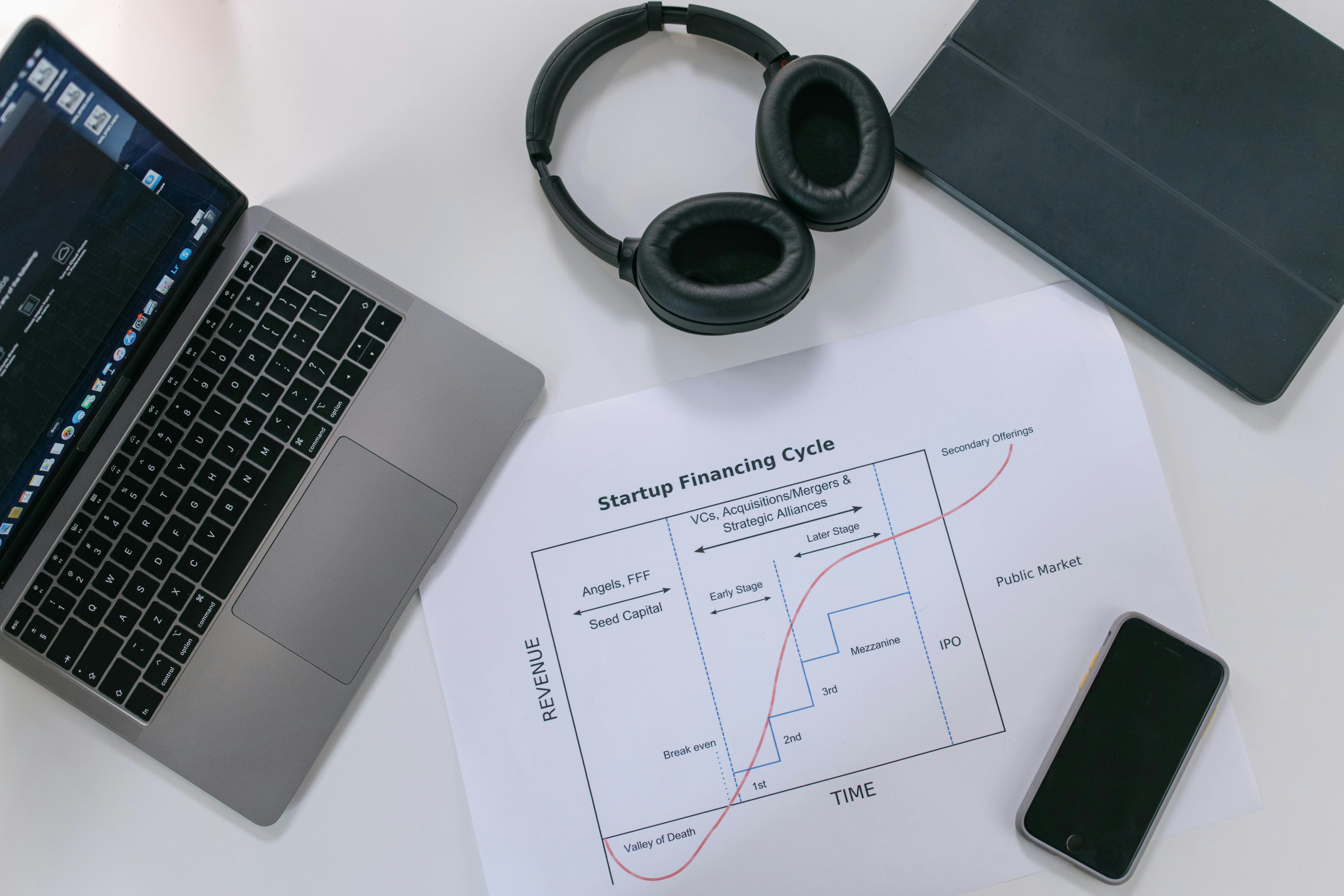
Beyond patient access, automation is a game changer for the financial side of healthcare. You can automate healthcare calls to payers and patients to accelerate revenue and reduce administrative waste.
Errors in patient data are a primary cause of claim denials. Manual insurance verification is tedious and error prone, with staff spending hours on the phone with payers. An AI agent can automate this by calling insurance companies, navigating their phone systems, and verifying benefits with near perfect accuracy. This includes eligibility checks to confirm active coverage before an appointment. This same technology can tackle prior authorization, another administrative burden, by initiating requests and following up on their status. Prosper AI’s agents can verify benefits with a less than 2 hour turnaround, ensuring clean claims from the start.
Many inbound calls are simple questions about bills. Automating billing and payment workflows for medical billing teams allows an AI agent to answer frequently asked questions, state a patient’s balance, and securely process payments over the phone. This provides patients with a convenient self service option and helps your organization collect payments faster. For more complex issues, the system can always offer a live agent escalation to a human billing specialist.
Implementing automation requires the right technology and a thoughtful approach. Here’s what makes a system effective, secure, and successful.
For automation to be truly effective, it needs to connect with your core systems. EHR and practice management integration allows an AI agent to read and write information directly into the patient’s record. This means an appointment scheduled by the AI appears instantly on the provider’s calendar, and a note about a billing inquiry is logged automatically. Without this connection, staff are left with manual data entry, defeating the purpose of automation.
Handling protected health information (PHI) requires ironclad security. Any solution you use must feature HIPAA compliant data security. This includes data encryption, secure access controls, and a signed Business Associate Agreement (BAA). With the average cost of a healthcare data breach hitting nearly $11 million, you cannot afford to compromise on security. When you automate healthcare calls, you must ensure your platform partner prioritizes patient privacy.
Modern AI enables a high degree of personalization.
Customizable Call Flows: A well designed system uses customizable call flows that can be adapted to your practice’s specific needs without complex engineering, ensuring the patient experience is logical and helpful.
Multilingual Support: To serve diverse patient populations, AI agents can offer multilingual support, communicating with patients in their preferred language. This improves understanding, builds trust, and ensures equitable access to care.
Omnichannel Strategy: While voice is a primary channel, a true omnichannel communication strategy integrates voice with text and email for things like reminders and follow ups, meeting patients where they are.
Getting started doesn’t have to be overwhelming.
Phased Implementation: Start small. A phased implementation allows you to test and refine the system with a limited scope before a full rollout.
Use Case Prioritization: Begin with your biggest pain point. Is it appointment scheduling backlogs or high call abandonment? Focus on the use case prioritization that will deliver the most immediate value.
Patient Flow Mapping: Before you automate, map your current processes. Understanding the existing patient flow mapping helps you design a better, more efficient automated workflow.
Once live, the work isn’t over. Continuous training for both AI models and human staff ensures the system improves over time. By using analytics and insights from call data, you can spot trends and find new opportunities for improvement. This data driven approach, supported by robust contact center KPI tracking (like hold time and first call resolution), turns your call center into a constantly learning operation. For complex calls the AI can’t handle, it seamlessly transfers to a person. This is called live agent escalation. For your human team, agent assist tools can provide real time information and suggestions, making them more effective. If you’re looking to begin your journey, a good first step is to get started with a demo to see how these tools work in a real world setting.
1. What is the first step to automate healthcare calls?
The best first step is to identify your biggest communication bottleneck. This could be long hold times for scheduling, high no show rates, or the staff hours spent on insurance verification. Start with a single, high impact use case.
2. Is AI voice automation secure for patient information?
Yes, provided you choose a reputable vendor. Look for platforms that are explicitly HIPAA compliant, offer a Business Associate Agreement (BAA), and have security certifications like SOC 2. They should use end to end encryption to protect all patient data.
3. Will patients be frustrated talking to an AI?
Modern conversational AI is far more natural and effective than old IVR systems. When an AI can resolve a patient’s issue quickly and efficiently (like scheduling an appointment in two minutes instead of waiting on hold for ten), patient satisfaction often increases. The key is a well designed system with the option to escalate to a human agent if needed.
4. How long does it take to implement an AI voice agent?
The timeline varies, but it can be surprisingly fast. With pre built workflows for common healthcare tasks, some organizations can go live with a simple automation in just a few days or weeks, especially when working with a specialized platform like Prosper AI.
5. Can AI handle calls with insurance companies?
Absolutely. This is a powerful use case for revenue cycle management. AI voice agents can call payers, navigate their automated systems, wait on hold, and even speak with human representatives to verify benefits, check on prior authorizations, or get claim statuses.
6. Does automation replace my front desk staff?
The goal is not to replace staff but to augment them. By letting AI handle routine, repetitive calls, you free up your skilled staff to focus on more complex patient needs and provide better in person care. It helps reduce burnout and makes their jobs more rewarding.
Discover how healthcare teams are transforming patient access with Prosper.

Evaluate HIPAA-compliant voice AI providers 2025: top 5 picks, security and SLA checklists, EHR integrations, KPIs, and rollout tips. Get the buyer’s guide.
Learn how to build HIPAA-compliant AI frameworks 2025 with BAAs, least-privilege, RAG, and zero retention. Get a clear, actionable roadmap. Download the guide.
Learn the full revenue cycle management process, from intake to coding, claims, denials, and patient billing—plus KPIs and AI tips. Boost cash flow today.