Revenue Cycle Management (RCM) explained end to end—front, mid, and back office. Reduce denials, speed cash flow, track KPIs, and leverage AI. Get 2026 guide.

Patients expect to book care like they book travel. Patient self scheduling software lets people find a time, confirm appointments, and receive reminders without waiting on hold. For clinics, it reduces abandoned calls, fills the calendar, and frees staff for higher value work.
The timing is right. Call volumes are rising, staffing is tight, and access targets are under pressure. Modern tools integrate with EHR and PM systems, verify eligibility in the background, and sync reminders over text and email. Some platforms pair self service with voice agents that answer and place calls, which closes the loop when a visit requires nuanced triage or payer follow up. If you need a fast path to value, explore Prosper AI’s voice first approach to patient access and RCM, including scheduling, reminders, benefits, and authorizations. See details and request a demo at Prosper AI.
Patient self scheduling software delivers measurable access and revenue gains when it is tied to the operational reality of your practice.
Use this quick checklist to confirm fit and reduce surprises.
Scheduling touches protected health information, so the solution and vendor must meet the bar.
When comparing patient self scheduling software, prioritize features that drive access and accuracy without extra work for staff.
Prosper AI brings several of these together in one platform. Agents schedule visits, call payers, write back structured results to EHR or PM systems, and surface analytics to your team. Learn more at Prosper AI.
Patient self scheduling software only works if it syncs with the systems you already use.
Building on the drivers we just covered, this section spotlights the top patient self-scheduling platforms clinicians actually use. These are tools that let patients book, reschedule, and check in without a phone call. We grouped these picks because they consistently balance patient convenience with operational gains like tighter provider utilization, fewer no-shows, and smoother EHR integration across practice sizes.
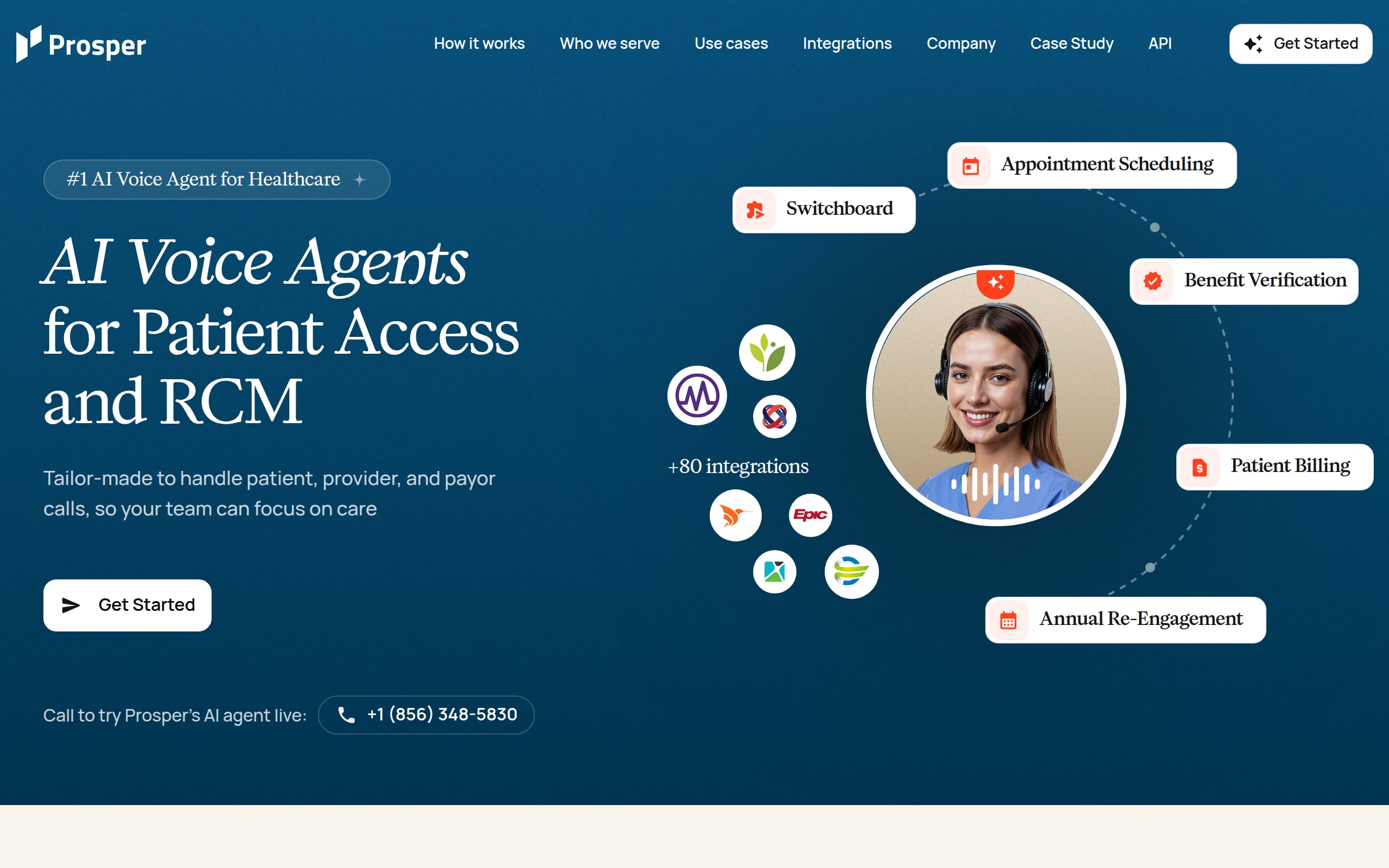
Prosper AI’s “Anna” is a healthcare-trained voice agent that answers patient calls around the clock and books, reschedules, or cancels directly in your EHR/PM. By removing hold times and capturing insurance on the same call, it boosts access, increases call containment, and helps cut no-shows.
Best for: Health systems, multi-specialty groups (OB/GYN, GI, derm), multi-location practices or DSOs with high inbound volume, overflow, or limited after-hours coverage, and for EHR/PM vendors adding voice scheduling for customers.
What you’ll get:
Buying snapshot: Usage-based pricing with volume tiers and enterprise SLAs. Deployments range from 1 to 2 days (file-based) to ~3 weeks (APIs/EHR). Voice-first strengths include after-hours coverage and call deflection; pair with portals if web booking is a must.
Dash by Relatient unifies self-scheduling, centralized scheduling, and AI voice/chat into a rules-driven access platform that works across mixed EHR ecosystems. The result: 24/7 online booking that deflects routine calls and drives measurable no-show reduction.
Best for: Hospitals and health systems, multi-specialty groups (orthopedics, GI, dermatology), and MSOs/PPMs managing complex provider rules, high call volume, and limited after-hours coverage.
What you’ll get:
Buying snapshot: Quote-based and modular pricing (providers/locations, messaging volume). API-led deployments typically ~90 days. Strengths include breadth of integrations and KLAS-validated leadership; trade-offs are rules configuration effort and higher enterprise pricing.
Built into NextGen Enterprise PM/EHR, this rules-based tool lets patients book, reschedule, or cancel in real time without requiring extra portals. With Luma-powered engagement, it adds waitlists and reminders to reduce call volume and lighten staff workload.
Best for: Ambulatory groups on NextGen Enterprise. This includes multi-specialty practices, FQHCs/CHCs, and high-volume, multi-location clinics (primary care, OB/GYN, behavioral health, ENT, GI, derm) seeking after-hours access and automated waitlists.
What you’ll get:
Buying snapshot: Sold as a NextGen Patient Experience add-on with quote-based pricing by module and footprint. Implementations for existing NextGen clients are typically light; AI, waitlist, and IVR/chatbot may be add-ons.
Experian Health’s omni-channel scheduler brings real-time booking to web, mobile, outbound outreach, and call centers. This tightens inventory control while deflecting calls and shortening handle times.
Best for: Multi-hospital systems, AMCs, and large multi-specialty groups managing centralized or distributed call centers, heavy referrals, and after-hours demand across many locations.
What you’ll get:
Buying snapshot: Quote-based pricing tied to scale, channels, and interface complexity. Expect front-loaded template/rules design with light training. Strengths include scale and Epic integration; validate non-Epic connectors and governance to avoid friction.
InteliChart’s Patient Schedule lets new and existing patients book in real time through customizable decision trees without requiring an app. Two-way EHR/PM sync mirrors provider rules to deflect calls and meet after-hours demand.
Best for: Ambulatory groups needing consumer-grade access aligned to clinical templates. It is ideal for multi-specialty practices (GI, derm, ortho), FQHCs/CHCs, and multi-location organizations with heavy call volume or thin after-hours staffing.
What you’ll get:
Buying snapshot: Modular, quote-based pricing. Deployments accelerate with existing EHR/PM integrations; telehealth can go live in ~48 hours. Strengths are bidirectional scheduling; trade-offs include pricing opacity and multi-module enablement.

CERTIFY Health’s Patient Self-Scheduling extends 24/7 online booking with real-time EHR sync, ASAP waitlist automation, and mobile/kiosk check-in, which shaves calls, cuts no-shows, and speeds access.
Best for: Health systems, hospitals, multi-site ambulatory groups, imaging centers, behavioral health, DSOs, and specialty clinics with high-volume primary/urgent care, multi-location coordination, and limited after-hours coverage.
What you’ll get:
Buying snapshot: Quote-based tiers (Essentials, Growth, Premier); self-scheduling typically starts in Growth. EHR go-live ~4–8 weeks. Strengths include unified access and deep compliance; verify API scope by tier, telehealth link specifics, and messaging/SLA terms.
Mend streamlines behavioral health access with 24/7 self-scheduling, configurable rules, and bidirectional EHR/PM sync, paired with link-based telehealth and engagement tools that have driven sizable reductions in no-shows.
Best for: Community mental health centers, outpatient psychiatry/therapy groups, CCBHCs, and FQHCs, especially multi-location teams with long waitlists, heavy telehealth, and limited after-hours staff.
What you’ll get:
Buying snapshot: Quote-based with ROI guarantee. Can launch without deep integration, though EHR sync unlocks full value. Excellent behavioral health fit; confirm Epic/Cerner integration depth and SSO. Outcomes hinge on configuration and practice policies.

PracticeQ (from IntakeQ) combines lightweight practice management with an embeddable booking widget so patients can schedule anytime. Automated reminders, integrated payments, and digital intake keep calendars full and phone tags to a minimum.
Best for: Solo and small-to-mid-size outpatient clinics (such as behavioral health, med spas/aesthetics, and direct primary care) needing quick deployment, after-hours booking, and simple multi-location support with lean front-desk teams.
What you’ll get:
Buying snapshot: Transparent, monthly pricing: Starter at $54.90 and Pro at $79.90 per practitioner, plus optional e-prescribe and payments fees. Setup is light (embed widget, set services, sync calendars). Limits include EHR connectors focused on intake/demographics and EasyFill in beta; confirm security documentation.

DrChrono’s mobile-first EHR/PM pairs an embeddable scheduling widget with the OnPatient portal so patients can book 24/7. Add digital check-in, reminders, and native telehealth to keep schedules full and reduce no-shows.
Best for: Small and midsize ambulatory practices and multi-specialty groups that favor an iOS-first workflow. It is especially suited for primary and urgent care needing self-booking and integrated telehealth.
What you’ll get:
Buying snapshot: Quote-based tiers (Prometheus, Hippocrates, Apollo, Apollo Plus) with training and migration options; reminder/faxing overages may apply. Setup is light-to-moderate. Strengths are native telehealth and eligibility; limitations include iOS-only provider app and no overlay for Epic/athena.

SimplePractice serves behavioral health with an intuitive practice platform where the Client Portal enables 24/7 appointment requests. Built-in confirmations and reminders extend after-hours access and help drive meaningful no-show reductions.
Best for: Solo and small-to-midsize behavioral health practices (therapy, counseling, and psychiatry) and growing groups wanting self-service intake with request-based scheduling.
What you’ll get:
Buying snapshot: Pricing (Mar 2025): Starter $49, Essential $79, Plus $99 monthly; groups add clinicians from $74 each. Self-serve setup with a 30-day trial; client import in 1 to 3 days. Strengths are speed and simplicity; limits include approval-based booking, plan-gated features, and no Epic/athena/Cerner integrations.
Getting from kickoff to impact requires clear ownership and tight feedback loops.
Define baseline metrics, then monitor weekly and monthly. Patient self scheduling software should show quick wins.
| Metric | Baseline | Target after 60 to 90 days |
|---|---|---|
| Call abandonment rate | Current level | Down 30 to 80 percent depending on channel mix |
| Average speed of answer | Current level | Near zero for self service with voice agent backup |
| No show rate | Current level | Down around 20 to 30 percent with reminders and easy reschedule |
| Appointments booked online | Current level | Up to a majority of eligible visit types |
| Staff time per appointment | Current level | Down significantly with automation and fewer callbacks |
| Denials linked to missing eligibility or authorization | Current level | Down with automated checks and faster follow up |
Prosper AI cites hundreds of thousands of calls across large health systems and partners, benefits verification and prior authorization SLAs under two hours with 99 percent accuracy, and claims follow up at 50 percent lower cost with 15 percent higher collections on denials. Pairing these capabilities with patient self scheduling software compounds the ROI. Prosper AI
Patient self scheduling software has moved from nice to have to essential. It improves access, reduces phone queues, and protects revenue when it is connected to eligibility, authorization, reminders, and live support. Look for a platform that integrates with your EHR, meets HIPAA and SOC 2 requirements, and offers fast deployment with measurable outcomes. If you want voice agents plus self service in one place, explore a demo of Prosper AI.
It is an online and phone enabled tool that lets patients book, confirm, and change appointments without waiting on hold. Leading platforms sync with the EHR calendar and trigger reminders and eligibility checks.
By sending timely reminders, offering quick rescheduling, and capturing pre visit tasks in advance. Prosper AI reports about 30 percent fewer no shows with scheduling agents and reminders. Prosper AI
Yes, leading tools collect demographics, insurance photos, and consent, then run eligibility checks automatically. If a visit needs an authorization, the system can start that workflow or hand it to a voice agent.
Vendors should sign a BAA, provide SOC 2 Type II reporting, encrypt data in transit and at rest, and support SSO and audit logs. Prosper AI lists these controls and offers cloud or on premises options. Prosper AI
With batch data and a narrow scope, pilots can launch in 1 to 2 days. Full EHR or API integrations typically take about 3 weeks based on Prosper AI guidance. Prosper AI
Track call abandonment, speed of answer, online booking rate, no show rate, staff time per appointment, and denials tied to eligibility or authorization misses.
No. It deflects high volume routine calls and pairs well with voice agents that handle complex cases and after hours coverage, which keeps access open and patients satisfied.
See use cases and request a demo at Prosper AI.
Discover how healthcare teams are transforming patient access with Prosper.

Revenue Cycle Management (RCM) explained end to end—front, mid, and back office. Reduce denials, speed cash flow, track KPIs, and leverage AI. Get 2026 guide.

Learn payer verification best practices to cut denials, speed reimbursement, and boost patient transparency. See steps and 2026-ready workflows you can use.

Learn how AI for Revenue Cycle Management automates prior auths, boosts clean claims, cuts denials, and accelerates cash flow. Get the 2026 guide and roadmap.