Revenue Cycle Management (RCM) explained end to end—front, mid, and back office. Reduce denials, speed cash flow, track KPIs, and leverage AI. Get 2026 guide.

Verifying coverage before care is the difference between clean claims and write-offs. Medical insurance eligibility verification software moves this work from phone calls and portal hopping to a reliable, auditable workflow that delivers answers fast and feeds your EHR or practice system automatically. This guide explains why it matters, what to buy, how to measure ROI, and how leading teams implement it. It also queues up the Top 10 Medical Insurance Eligibility Verification Software Solutions list for easy vendor research.
Eligibility mistakes show up later as denials and delayed cash. Industry data has consistently found that registration and eligibility issues are a top driver of denials, accounting for nearly 27 percent in some studies, and roughly half of denials stem from front end problems. (mgma.com)
Modern medical insurance eligibility verification software automates high volume checks, standardizes data capture, and returns structured benefits to schedulers and billers so visits start clean and claims go out right the first time.
Manual work means long payer hold times, IVR mazes, and inconsistent notes. For many specialties, a single manual eligibility check by phone or fax can take about 24 minutes and cost around 14 dollars in staff time per transaction. (caqh.org)
Even when staff use payer portals, rules differ by plan and benefit type. Without normalized outputs, teams rekey the same data into multiple systems, which compounds error rates and slows downstream processes.
Rising denials are a reality for many providers. Nearly half of organizations reported higher denial rates in 2023 and errors in patient access and registration ranked at the top of initial denial reasons. (acdis.org)
The financial stakes are significant. Some reports noted denials rising to about 11 percent of all claims and the dollar value of denials increasing sharply in 2022, which strained margins and added rework. (healthleadersmedia.com)
Granular analyses also place eligibility as a recurring top reason across professional and inpatient claims at around 17 percent, with measurable impact on outpatient claims as well. (nahri.org)
Electronic eligibility and benefits verification has long been supported by HIPAA transactions. CMS operates the Medicare HETS service for X12 270 and 271 real-time eligibility checks and notes that HETS is real-time only and does not accept batch transactions. (cms.gov)
The No Surprises Act adds obligations for accurate cost visibility. Since January 1 2022 most providers must furnish a good faith estimate for uninsured or self pay patients within specific timeframes such as within one business day when a service is scheduled at least three business days out or within three business days upon request. (cms.gov)
CMS also finalized the Interoperability and Prior Authorization rule in January 2024 that pushes payers toward FHIR based APIs for data exchange and prior authorization. Compliance timelines generally begin in 2026 for operations and 2027 for API requirements. (cms.gov)
Eligibility verification underpins these requirements because accurate coverage and benefits data feed patient estimates, authorizations, and cleaner claims.
The case is straightforward. Medical insurance eligibility verification software reduces time per check, cuts variation across staff, and writes structured outputs back to your EHR or PM system. CAQH estimates show billions in savings opportunities when organizations move eligibility and claim status to fully electronic workflows. (caqh.org)
Success typically looks like:
Fewer first pass denials tied to eligibility
Shorter registration and scheduling handle times
Accurate patient financial estimates that reduce surprise bills
Clean claim rates that trend up and faster days in A R
If your team still calls payers when portals fall short, consider voice AI that can wait on hold and capture up to dozens of benefit data points then post results to your system. That is where platforms like Prosper AI can complement medical insurance eligibility verification software with payer phone automation and near real-time structured outputs to your EHR or PM.
Prioritize features that map to your highest volume workflows and payer mix:
Broad connectivity, support for X12 270 and 271, payer portals, clearinghouses, plus APIs or SFTP
Phone automation for edge cases where portals lack detail or are down
Normalized outputs, patient responsibility, copay, deductible, accumulators, plan limitations, visit or procedure-specific rules
Deep plan and benefit logic, multiple coverage tiers, secondary and tertiary plans
Real-time status with audit trails and call or transaction transcripts
Seamless EHR or PM integration, Epic, athena, Cerner, MEDITECH, NextGen, and more
Embedded QA, accuracy scoring, and analytics by payer, plan, and facility
Enterprise security, HIPAA with BAA, SOC 2, encryption, role based access, SSO
Deployment options that fit IT policies, cloud or on premises
Human in the loop exception handling
If your operations include both portal checks and payer calls, a combined approach with AI benefits verification can cover gaps and maintain a two‑hour or better turnaround for phone‑based verifications.
Use this fast checklist when shortlisting medical insurance eligibility verification software:
Workflow fit, does it support your specialties, benefits, and multi plan logic
Payer coverage, which plans are electronic only and which are supported by phone automation
Accuracy and SLA, ask for audited QA results with sampled call or transaction reviews
Integrations, confirm certified connections to your EHR or PM and your clearinghouse
Security posture, HIPAA with BAA, SOC 2, encryption at rest and in transit, SSO
Data handling, retention periods, on premises or zero retention LLM options if using AI
Reporting, denial trending by reason, throughput, and staff productivity metrics
Reference calls, similar size and specialty customers
Implementation plan, roles, training, and a realistic three to six week timeline to production
Vendors that offer AI voice agents to call payers can show transcripts, captured data points, and QA scoring on every call. Ask providers like Prosper AI for side by side comparisons versus manual staff calls.
Model the value in simple terms that finance will trust.
Inputs
Current manual checks per month
Average minutes per manual check and fully loaded labor rate
Denial rate due to eligibility and average reimbursement per claim
Rework cost per denial, follow up time and appeals
Software and telephony costs
Example levers to quantify
Time saved per check when moving from phone or portal to electronic workflows and automation, CAQH analyses show double digit minute reductions per transaction across common admin processes. (caqh.org)
Denial reduction, eligibility related denials have been measured in the teens to upper twenties percent of denials, so even modest reductions drive material cash. (mgma.com)
Faster estimates and scheduling throughput that reduces no shows and cancellations
Track these KPIs
Eligibility cycle time
First pass yield and denial rate by reason code
Days in A R and cost to collect
Patient estimate accuracy and patient pay conversion
Staff productivity per thousand verifications
A smooth rollout blends process, people, and technology.
Map your top visit types and benefits, include high dollar imaging, surgery, and infusion
Standardize data capture, define required fields and naming conventions
Start with a pilot location or specialty, then scale by payer or region
Integrate early with your EHR or PM so results post directly into the scheduling and billing workflow
Train schedulers and billers on exception handling and escalation paths
Set weekly QA reviews, sample transactions and calls, and publish scorecards
Build a denial feedback loop, adjust rules based on actual payer responses
For phone‑heavy payers, pair your core platform with Prosper AI voice agents that can navigate IVRs, wait on hold, and talk to representatives, then write back structured benefits
Now that we’ve outlined what effective eligibility checks require, this section spotlights the tools built to do that work at scale. These ten platforms are grouped for their strong payer connectivity, real-time 270/271 capabilities, automation that reduces manual touches, and measurable impact on denials and staff workload. Use this shortlist to quickly compare strengths and match solutions to your practice size, specialty mix, and budget.
Alex is a voice AI agent that calls payers, navigates IVRs, talks to reps, and writes structured benefits straight into your EHR/PM when 270/271 or portals fall short. It slots into front‑end access or centralized verification and shines for health systems, multi‑specialty groups, and billing firms.
What stands out
Real‑time and batch verification with sub‑two‑hour phone turnaround.
Complements clearinghouses/APIs/portals by automating phone/IVR outreach 24/7.
Captures deep details: copays, deductibles, coinsurance, effective dates, COB, secondary.
Flags prior auth; supports claim status/EOB follow‑ups into RCM queues.
Rules, Battle-tested Blueprints, QA; full recordings, transcripts, dashboards, and productivity analytics.
80+ EHR/PM connections (Epic, athenahealth, eClinicalWorks, NextGen, MEDITECH, AdvancedMD).
APIs, SFTP, SSO; HL7/FHIR via EHR connectors for bidirectional updates.
Results you can expect
Reported 50% cost reduction, 99% accuracy, and sub‑two‑hour SLA.
Faster pre‑registration; fewer preventable denials via complete benefits capture.
Significant staff hours saved and hold time avoided; higher throughput.
Rapid go‑live: 1–2 days via SFTP; ~3 weeks for deeper integration. See real‑world outcomes in our case studies.
Security, compliance & data handling
HIPAA + BAA; SOC 2 Type II/HITRUST; encryption at rest/in transit; audit logs; PHI retention controls; cloud/on‑prem; SSO.

Experian Health streamlines real‑time and batch 270/271 checks through eCare NEXT and OneSource, clearing patients up front and propelling clean claims downstream. It fits front desk and centralized verification, ideal for health systems, large multi‑specialty groups, and enterprise billing partners running Epic/Cerner‑aligned workflows.
What stands out
Real‑time and batch eligibility via eCare NEXT, OneSource, and X12 270/271.
900+ payer connections; portal enrichment cushions outages.
Rich 271 benefits: deductibles, coinsurance, copays; COB/secondary coverage.
Prior auth and medical necessity flags through Experian Authorizations.
277 claim status blended with portal data to drive worklists.
Exception‑based rules, alerts, and dashboards enable touchless pre‑reg; no IVR.
Deep EHR/PM integrations: Epic, Oracle Health, MEDITECH, athena.
APIs, X12, HL7/FHIR, and SSO for enterprise‑grade pipelines.
Results you can expect
Providence cut denial exposure by $18M in five months.
Best Possible Coverage uncovers ~$30M annually.
MLK Community shaved two to three minutes off most registrations.
MBI Lookup resolves 60% of missing Medicare IDs, accelerating reimbursement.
Security, compliance & data handling
HIPAA + BAA; HITRUST; SOC 2 Type II; PCI DSS; encryption; audit logs; monitoring; PHI retention; cloud/on‑prem.

AdvancedMD’s eEligibility brings real‑time and scheduled benefits checks into native scheduling and insurance tabs, so front‑desk and centralized teams resolve coverage before arrival. It’s built for independent practices, multi‑specialty groups, and billing firms on AdvancedMD (not large Epic/Cerner health systems).
What stands out
Real‑time eligibility and batch sweeps for upcoming appointments.
EDI 270/271 connectivity plus per‑payer portal credentials as needed.
Benefits depth: deductibles, copays, coinsurance, COB, secondary coverage.
ePA for prescriptions; roadmap for broader medical prior auth.
Claim status via nightly batches or on‑demand inquiries.
Rules, alerts, dashboards, task queues, and write‑backs streamline follow‑ups.
Native to AdvancedMD PM/EHR; partners (e.g., pVerify) extend estimation.
Connect APIs, FHIR R4/SMART, SAML SSO, ODBC; HIE‑friendly.
Results you can expect
Fewer eligibility denials and less front‑desk rework.
About 16 minutes saved per verification versus manual calls (benchmarks).
Lower per‑check costs; better throughput for specialists.
Instant on‑demand checks; batch after required enrollments.
Security, compliance & data handling
HIPAA/BAA; encryption in transit and at rest; audit logs; AWS hosting; DR; 271 retained ~30 days.
iCoreVerify automates real‑time and pre‑visit eligibility across the schedule so staff confirm benefits before patients arrive. It’s purpose‑built for dental RCM and is best for solo practices, DSOs, and billing firms. Medical ambulatory use is limited and it isn’t hospital‑grade.
What stands out
Real‑time checks and seven‑day pre‑visit sweeps.
2,100+ payer connections; Plus/Pro tiers complete verifications end‑to‑end.
No IVR bot; concierge staff handle payer calls when needed.
Dental‑specific benefits: deductibles, frequencies, annual maximums, remaining benefits; Pro chart‑posts.
Focused scope: no dedicated prior auth module.
Claim status via companion iCoreClaims.
Rules, flags, unscheduled‑treatment prompts; dashboards in iCoreAnalytics.
Integrates with dental PMs; medical EHRs unlisted; no HL7/FHIR/APIs/SSO.
Results you can expect
80 to 90% automation; Plus/Pro approaches near‑100% completion.
Saves 50+ staff hours monthly; 3× faster with ~99.9% accuracy.
Pre‑visit sweeps shorten check‑in and curb denials.
Unlimited‑verification pricing; deployments in days with training.
Security, compliance & data handling
HIPAA/HITECH + BAA; SOC 2; AES‑256 encryption; audit logs; US‑based support; cloud/SaaS; PHI retention not specified.
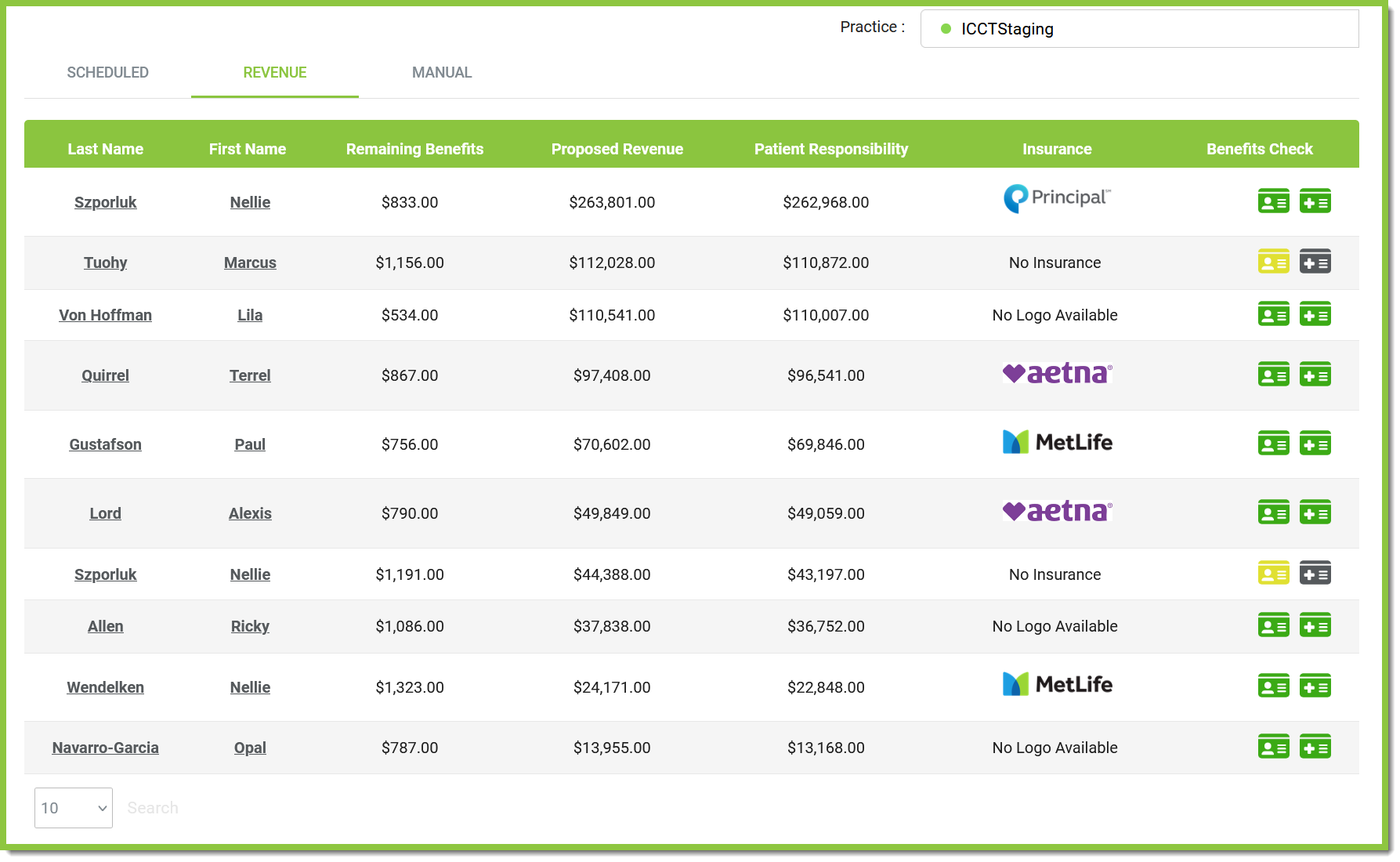
maxRTE marries Insurance Discovery with real‑time eligibility, enabling pre‑reg batch sweeps and one‑click point‑of‑service checks inside major EHRs or a web portal. It’s a strong fit for hospitals, health systems, multi‑site clinics, and high‑volume billing firms that favor flat‑rate pricing and centralized ops.
What stands out
Real‑time and batch eligibility via SFTP plus POS workflows.
Discovery locates primary/secondary/tertiary coverage across major payers.
1,000+ payer links; CAQH CORE‑certified 270/271; X12 rails.
Detailed benefits: copays, coinsurance, deductibles, coverage, effective dates.
Prior auth detection, automation, tracking, and alerts.
276/277 claim status; depth varies by payer.
Rules, work queues, dashboards, Discovery ROI reporting.
Integrations: Epic, Cerner, athenahealth, MEDITECH; APIs, HL7, FHIR; no IVR.
Results you can expect
Up to 25% of self‑pay accounts converted via discovered coverage.
As much as 25% reduction in eligibility‑related denials.
30% staff workload reduction; faster pre‑reg and scheduling.
Go‑live in hours; case studies cite 34× ROI and $2.9M–$3.47M recovered.
Security, compliance & data handling
HIPAA + BAA; SOC 2 Type II; CAQH CORE; DirectTrust/EHNAC; encryption in transit/at rest; audit logs; SaaS.

Coverage Insight uncovers undisclosed active coverage and verifies it with payers, then feeds confirmed results into eligibility and benefits workflows. Deployed alongside real‑time 270/271, it supports front‑end access and centralized verification, making it well-suited to hospitals and health systems managing sizable self‑pay volumes.
What stands out
Coverage discovery for self‑pay/underinsured across Medicare, Medicaid, and commercial sources.
Identity‑risk suppression trims false positives and PHI exposure; ~40% risky profiles suppressed.
Hit‑rate signals: 12–14% uninsured hit rate at ~90% billability.
Medicaid COB screening finds primaries, preventing COB denials.
Consolidated callback pairs RTE 270/271 with discovery in one payload.
EHR/PM connectivity via 270/271, HL7; APIs with OAuth2/TLS and queueing.
Prior auth and claim status APIs plug into unified clearance.
Results you can expect
Discoveries within 24 hours reduce bad debt and speed conversion.
12–14% uninsured hit rate at ~90% bill rate improves net yield.
$280M reimbursement found in 2023; programs clear ~$800M annually.
COB detection prevents downstream denials; fewer portal logins and calls.
Security, compliance & data handling
HIPAA + BAA; encryption at rest/in transit; audit logs; PHI retention controls; cloud SaaS; SOC 2/HITRUST attestations on request.

Inovalon’s Insurance Discovery finds active, billable coverage for self‑pay or incomplete registrations and runs alongside Eligibility Workflow and Registration Assurance in myABILITY. It supports front‑end access, centralized teams, and even back‑end cleanup, for health systems, SNFs, multi‑specialty groups, billing firms, and payers.
What stands out
Real‑time and batch eligibility with re‑checks and weekly change alerts.
All‑payer discovery, demographic verification, coverage‑type detection, MBI retrieval.
Connectivity via clearinghouse rails, CMS HETS 270/271, and commercial/Medicaid portals.
271 benefits include plan status, copay, deductible, coinsurance (depth varies).
Prior auth indicators when present; no dedicated module.
Claim status EDI 276/277, edits, and ERA posting downstream.
Worklists, rules, dashboards in Eligibility Workflow/Registration Assurance; no IVR.
Integrations with Epic; APIs, X12/HL7/FHIR, and enterprise SSO.
Results you can expect
Faster pre‑registration with fewer portal hops and calls.
Up to 99% first‑pass acceptance when paired with Inovalon claims.
Automated re‑checks and alerts save staff hours and boost throughput.
Quick deployment via myABILITY and EHR marketplaces; fewer write‑offs.
Security, compliance & data handling
HIPAA + BAA; SOC 2/HITRUST; encryption in transit/at rest; audit logs; PHI retention controls; access management; cloud SaaS.
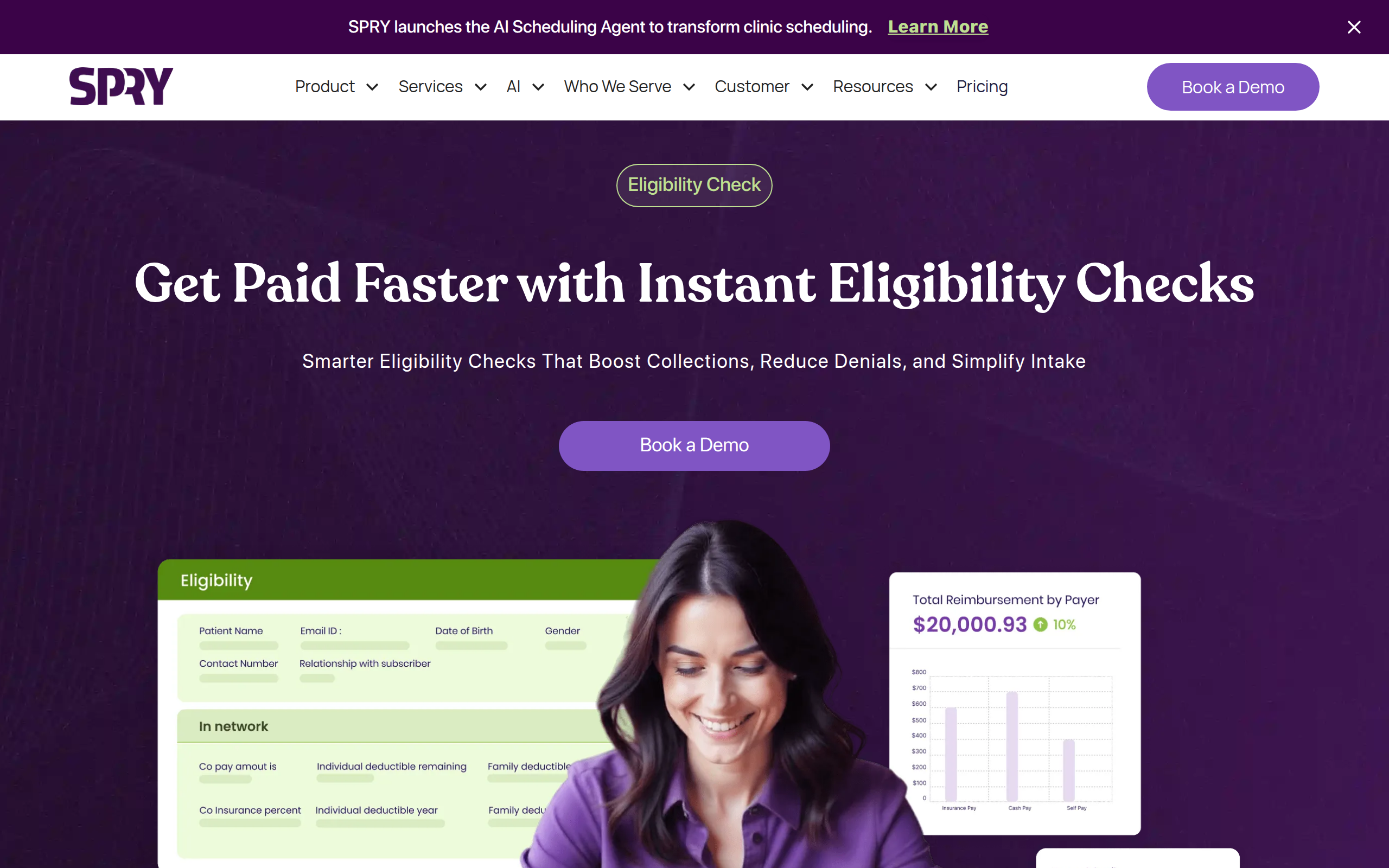
Spry automates eligibility and benefits at scheduling and pre‑reg, surfacing coverage, patient costs, visit limits, and prior‑auth needs without portal hopping. It’s a natural fit for front‑desk and centralized teams (or Spry RCM) across outpatient rehab, multi‑site practices, and billing groups seeking predictable workflows.
What stands out
Real‑time and nightly batch eligibility; 99% processed within an hour; 95%+ match.
Connectivity via clearinghouses, APIs, and payer portals for Medicare, Medicaid, and workers’ comp.
Phone/IVR automation trims hold time and queues exceptions.
Deep benefits: copays, deductibles, coinsurance, OOP max, visit caps/remaining visits, COB, secondary.
Prior‑auth detection with form assembly, submission, tracking, renewals, and alerts.
Claim‑status EDI tie‑ins, denial dashboards, and analytics.
Rules engine, queues, audits for consistent throughput.
Integrations with Spry, Epic, athena; FHIR/HL7/SSO APIs.
Results you can expect
95%+ eligibility match; 99% processed within an hour.
30% higher copay collections and 3× payment compliance.
Up to 40% fewer denials via upfront checks.
10–15 minutes saved per verification; prior auth 80% automated and 95% faster.
Security, compliance & data handling
HIPAA + BAA; SOC 2/HITRUST; encryption at rest/in transit; audit logs; PHI retention; cloud or on‑prem; SSO.

Change Healthcare’s EDI suite (ConnectCenter, iEDI, and APIs) powers real‑time 270/271 and batch pre‑reg across front desks, centralized verification, and RCM teams. It fits health systems, multi‑specialty groups, and billing firms, and it also supports payers hosting eligibility and claim‑status services within its clearinghouse.
What stands out
Real‑time and batch 270/271 via portal, clearinghouse, and APIs.
Broad payer connectivity with enrollment tooling and routing updates.
Benefits depth: deductibles, copays, coinsurance, limitations, network, effective dates.
Prior auth detection with 278 inquiry/submission options.
276/277 claim status tie‑ins plus hosted payer EDI services.
Rules, work queues, dashboards, and denial‑prevention KPIs.
EHR/PM integrations: Epic, eClinicalWorks, athena, and clearinghouse interfaces.
REST/JSON, X12, HL7/FHIR APIs; OAuth2 SSO via One Healthcare ID.
Results you can expect
Up to 99% clean claims when eligibility and edits run upstream.
Eligibility‑related denials drop via normalization and payer‑specific checks.
Real‑time 270/271 reduces portal hopping and phone hold time.
Rapid onboarding: API sandbox immediately; production after enrollments/testing.
Security, compliance & data handling
HIPAA + BAA; SOC 2/HITRUST; TLS encryption; key management; audit logs; PHI retention controls; cloud/SaaS.
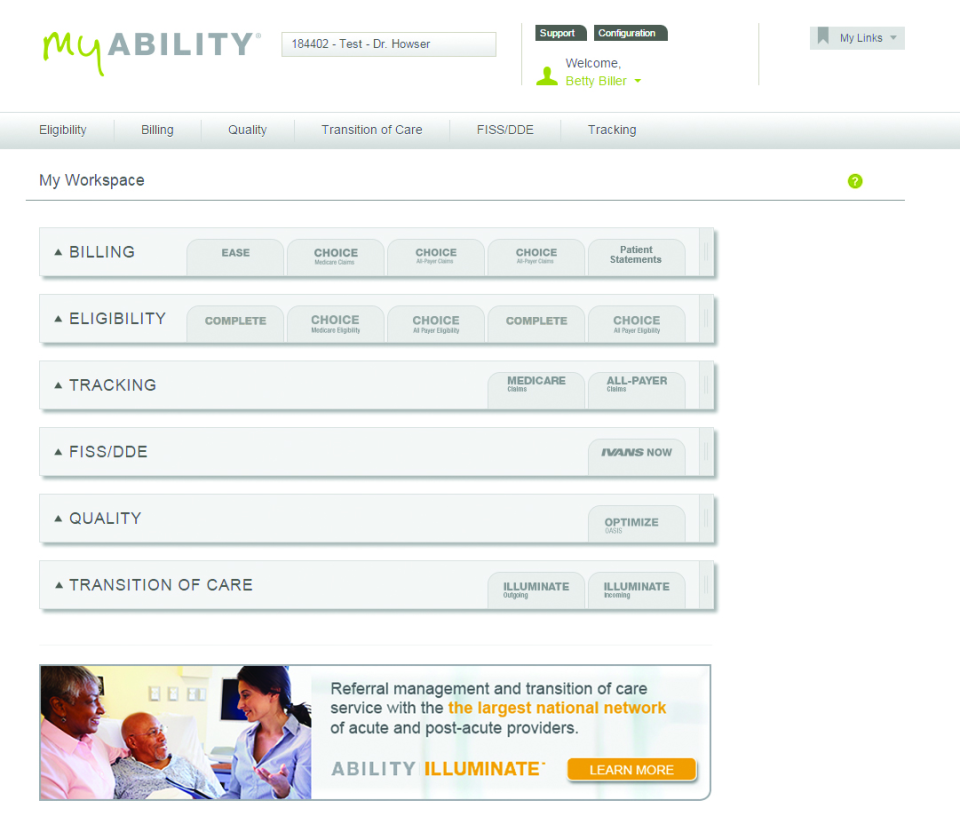
Provider Cloud, delivered via myABILITY modules like Registration Assurance and ABILITY/COMPLETE, verifies eligibility and benefits during pre‑reg and registration to feed cleaner claims. It serves front‑desk, centralized verification, and RCM teams across health systems, ambulatory groups, hospitals, and billing services organizations.
What stands out
Real‑time 270/271 and scheduled batch uploads with alerts.
All‑payer connectivity via clearinghouse rails, payer APIs, and portals.
No native IVR; verification relies on EDI/portals with vendor exceptions.
Returns copay, deductible, coinsurance, OOP max; supports COB/secondary discovery.
Prior‑auth likelihood flags; ties into 276/277 claim‑status workflows.
Configurable rules, work queues, dashboards, and performance analytics.
Integrations with Epic and PointClickCare; complements athena, Cerner, others.
API‑enabled SaaS; SSO supported; HL7/FHIR on request.
Results you can expect
Up to 99% first‑pass acceptance with eligibility rules enabled.
Faster pre‑reg via automated identity and coverage confirmation.
Staff efficiency from batch checks, single login, and fewer payer calls.
Rapid cloud deployment; scalable for enterprise operations.
Security, compliance & data handling
HIPAA + BAA; SOC 2/HITRUST; encryption at rest/in transit; audit logs; PHI retention controls; cloud SaaS.
Eligibility is converging with interoperability and prior authorization. CMS now requires impacted payers to stand up FHIR based APIs for patient, provider, and payer to payer data exchange and a dedicated prior authorization API, with most API requirements taking effect in 2027. (cms.gov)
Enforcement discretion also gives covered entities flexibility to use an all FHIR prior authorization API without X12 278, which signals a broader move toward modern API based workflows. (cms.gov)
Expect medical insurance eligibility verification software to expand into omnichannel verification that blends X12, APIs, portals, and AI voice calls so teams get complete benefits in one place. Medicare HETS remains a reliable real time source for Medicare eligibility, typically available around the clock with published downtime notices. (cms.gov)
Eligibility is not just a check box. It is the front door to clean claims, accurate patient estimates, and fewer write offs. Teams that adopt medical insurance eligibility verification software and pair it with smart phone automation reduce denial risk, speed up scheduling, and give patients clearer costs. If you want to see how payer phone work and electronic checks come together in one platform, visit Prosper AI or get started.
It is software that confirms a patient’s active coverage and benefits with a health plan, returns structured benefit details, and posts results into your EHR or PM. Many platforms also handle secondary coverage and accumulators.
By validating coverage and benefits before care, staff catch plan issues, authorizations, and non covered services early. Industry sources show eligibility related errors are a frequent cause of denials, so prevention pays off. (mgma.com)
Yes for edge cases and payers without robust electronic data. Some vendors use AI voice agents to call payers, wait on hold, and gather structured benefits automatically, which can be paired with your core medical insurance eligibility verification software. See Prosper AI.
Yes. Accurate eligibility and benefits feed estimates required under the No Surprises Act for uninsured or self pay patients and help meet the one to three business day timeframes. (cms.gov)
Common standards include X12 270 and 271 for eligibility and FHIR based APIs where available. CMS HETS supports real time Medicare eligibility transactions. (cms.gov)
Smaller pilots can stand up in weeks if you start with your highest volume visit types and payers. Ask vendors about prebuilt EHR or PM integrations and a clear project plan. For phone heavy payers, combine your core platform with Prosper AI to accelerate results.
Track eligibility cycle time, first pass yield, denial rates by eligibility reason codes, staff minutes saved per check, and estimate accuracy. Use weekly QA samples and publish scorecards to sustain improvements.
Discover how healthcare teams are transforming patient access with Prosper.

Revenue Cycle Management (RCM) explained end to end—front, mid, and back office. Reduce denials, speed cash flow, track KPIs, and leverage AI. Get 2026 guide.

Learn payer verification best practices to cut denials, speed reimbursement, and boost patient transparency. See steps and 2026-ready workflows you can use.

Learn how AI for Revenue Cycle Management automates prior auths, boosts clean claims, cuts denials, and accelerates cash flow. Get the 2026 guide and roadmap.